Learn to assess fall risk in nursing and prevent patient falls. Pass NCLEX safety questions. Keep patients safe.
Understanding Fall Risk in Nursing
Fall risk in nursing means how likely a patient is to fall. This is critical. Falls are the most common hospital injury.
Why this matters:
- Falls cause broken bones
- Falls cause head injuries
- NCLEX tests fall prevention often
- Preventing falls shows good judgment
Practice now:
Quick Risk Chart
| Risk | Who | Example |
|---|---|---|
| Low | Young, healthy | 25-year-old after surgery |
| Moderate | Uses crutches | 36-year-old with broken leg |
| High | Older, dizzy | 63-year-old with heart disease |
| Very High | Elderly who faints | 75-year-old who faints often |
NCLEX Tip
Highest risk = elderly patient who faints.
Pick safety first.
Learn more:
How to Assess Risk
Check these six areas.
1. Vital Signs
Check vitals:
- Check BP lying down
- Check BP standing
- Watch for dizziness
- Note heart rate changes
- Document changes
Practice:
2. Walking Ability
Check mobility:
- Does patient use walker?
- Does patient use cane?
- How is balance?
- Recent surgery?
- Can they walk alone?
- Is muscle strength good?
Study:
3. Medications
High-risk drugs:
- Sleeping pills
- Pain medications
- Blood pressure pills
- Heart medications
- Water pills
- Anti-anxiety pills
Review:
4. Mental Status
Check thinking:
- Is patient confused?
- Are they impulsive?
- Do they understand safety?
- Are they oriented?
- Do they follow instructions?
Learn:
5. Bathroom Needs
Check elimination:
- Urgent urination
- Frequent trips
- Nighttime bathroom use
- Can't hold urine
- Taking water pills
Practice:
6. Room Safety
Check environment:
- Any clutter?
- Good lighting?
- Safe shoes?
- Call bell close?
- Bed height OK?
- Floor hazards?
Study:
Tools: Morse Fall Scale | Assessment Guide
Fall Risk in Nursing: What to Do
Match your actions to risk level.
Low Risk
Basic steps:
- Teach call bell use
- Keep water nearby
- Clear walkways
- Turn on lights
- Give non-slip socks
- Show room layout
Related:
Moderate Risk
Add these steps:
- Use gait belt
- Place near nurse station
- Bathroom every 2 hours
- Review meds
- Encourage help
- Watch closely
Practice:
High Risk
More protection:
- Turn on bed alarm
- Check every hour
- Help with transfers
- Post fall risk sign
- Call physical therapy
- Apply yellow bracelet
- Lower bed
Study:
Very High Risk
Maximum safety:
- One nurse watches (1:1)
- Low bed with mats
- Room near station
- Hold team meetings
- Watch constantly
- Family at bedside
Learn:
Guidelines: CDC Prevention | Joint Commission
High-Risk Medications
Know these drugs.
Common Drugs
These increase risk:
- Sleeping pills - drowsiness
- Opioids - dizziness
- BP medications - low BP
- Heart pills - BP drops
- Diuretics - frequent urination
- Anxiety pills - sedation
- Psychotic pills - poor coordination
Safety Tips
Stay safe:
- Give at safe times
- Teach slow standing
- Watch first dose
- Tell doctor concerns
- Monitor side effects
- Review drug lists
Study more:
- Medication Giving
- Drug Side Effects
- Elderly Drug Safety
- Medication Lists
- Drug Combinations
- How Drugs Work
- ISMP Guidelines
Documentation
Write these details.
What to Write
Include:
- Risk score number
- Why at risk
- What you did
- Patient response
- What you taught
- Understanding checked
- Plan updates
Sample Note
"Fall risk assessment done. Morse score 55 (high risk). Age 78. Gets dizzy standing. Takes BP meds. Fell last month. Actions: bed alarm on. Yellow bracelet on. Non-slip socks on. Call bell in hand. Taught: call before getting up. Patient says 'I will call.' Will check hourly."
Charting help:
Patient Teaching
Teach these points.
Key Points
Teach patients:
- Call for help - every time
- Wait for nurse - don't rush
- Safe shoes - non-slip
- Clear path - no clutter
- Stand slowly - sit first
- Report problems - dizziness, weakness
- Use devices - walker, cane
- Bathroom safety - grab bars
Family Help
Include families:
- Show safe walking
- Remind about call bell
- Keep room neat
- Explain alarms
- Stay during high-risk times
Teaching help:
- Patient Teaching
- Communication
- Health Understanding
- Teach-Back Method
- Family Teaching
- Cultural Care
- Going Home Plans
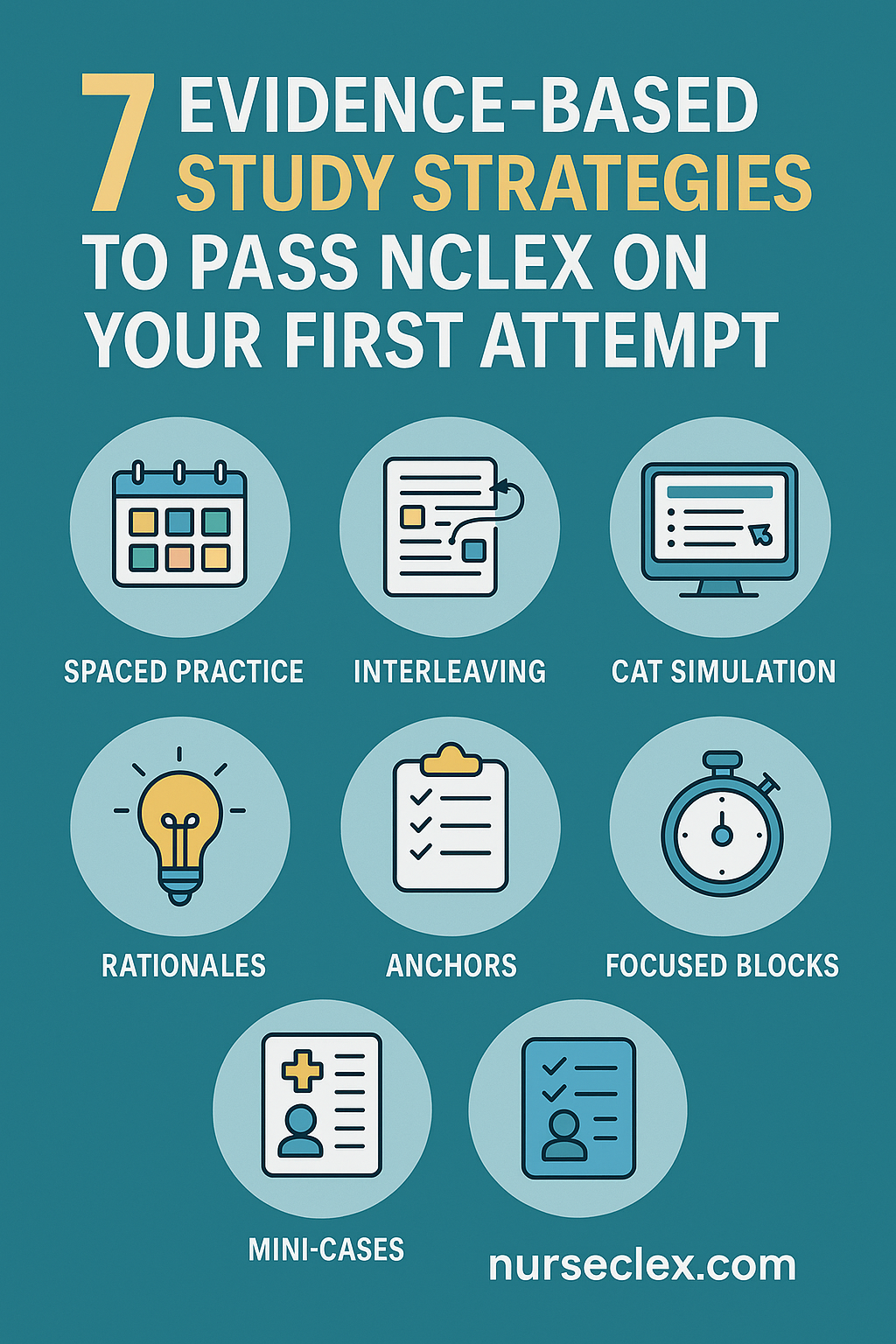
NCLEX Tips
Master test questions.
Key Rules
Remember:
- Safety beats comfort
- Elderly + fainting = top priority
- Dizzy after med = check vitals
- First walk = gait belt needed
- Safety always first
Common Questions
Question 1: Patient on BP med feels dizzy standing.
Answer: Sit patient down. Check vitals. Check BP lying and standing. Call provider. Don't let walk yet.
Related: Low Blood Pressure | Heart Care
Question 2: 75-year-old faints often. Wants bathroom alone.
Answer: Watch constantly (1:1). Bathroom every 2 hours. Bed alarm on. Low bed. Teach safety.
Related: Fainting Care | Seizure Safety
Question 3: Post-op patient on pain meds. Ready to walk first time.
Answer: Use gait belt. Sit on bed edge first. Safe shoes on. Stay with patient.
Related: After Surgery Care | Pain Management
NCLEX prep:
Case Studies
Practice with real cases.
Case 1: High Risk
Patient: 63-year-old on heart meds. Feels lightheaded standing.
Your action: Sit down. Check vitals. Check BP lying and standing. Call provider. Update plan.
Related: Heart Care | Chest Pain Care | Heart Medications
Case 2: Very High Risk
Patient: 75-year-old faints often. Walking to bathroom alone.
Your action: Watch constantly (1:1). Scheduled toileting. Bed alarm on. Low bed with mats. Teach safety.
Related: Fainting Care | Seizure Safety | Brain Emergencies
Case 3: Moderate Risk
Patient: 36-year-old. Broken leg. New crutches.
Your action: Teach crutches. Clear room. Safe shoes. Check pain med timing. Walk with patient.
Related: Broken Bone Care | Pain Management | Bone Care | Cast Care
More practice: Case Studies | Clinical Scenarios
Daily Workflow
Follow these steps.
Seven Steps
- Assess - Check risk
- Score - Use tool
- Plan - Pick actions
- Do - Apply safety steps
- Teach - Educate
- Document - Write it down
- Reassess - After changes
When to Reassess
Check again when:
- New meds start
- After procedures
- Status changes
- Patient falls
- Mobility changes
- Each shift
- Planning discharge
Skills practice:
Practice with Nurseclex
Master fall prevention.
Study Tools
Get:
Start now: Questions • Tests • Sheets
Key Points
Remember:
- Assess every patient
- Match actions to risk
- Elderly + fainting = highest priority
- Many meds increase risk
- Safety always first
- Document everything
- Teach prevention
- Reassess with changes
Keep learning: More at Nurseclex.com