Why NCLEX Fundamentals matters
NCLEX Fundamentals tests the core of safe, patient-centered care. Expect heavy emphasis on safety, infection control, basic care and comfort, vital signs, documentation, patient education, and delegation. Use the checklists below to anchor your review and practice NCLEX-style questions regularly.
Safety & Infection Control (NCLEX Fundamentals)
Standard precautions (for every patient)
-
Hand hygiene before/after contact
-
Gloves for contact with blood/body fluids
-
Mask/eye protection if splash risk
Transmission-based precautions
-
Contact (e.g., C. diff, MRSA): gloves + gown; dedicated equipment
-
Droplet (e.g., influenza, pertussis): surgical mask; 3+ ft distance
-
Airborne (e.g., TB, measles, varicella): N95 + negative-pressure room; limit transport
Fall prevention
-
Call light in reach; bed low & locked
-
Non-slip socks; clear pathways; good lighting
-
Bed/chair alarms for high-risk patients
Fire safety
-
RACE: Rescue → Alarm → Contain → Extinguish
-
PASS: Pull → Aim → Squeeze → Sweep
Restraints (last resort)
-
Provider order; time-limited
-
Check circulation q15–30 min; hydrate/toilet/comfort
-
Remove ASAP; document reason, checks, and response
Basic Care & Comfort
Positioning
-
Fowler’s (45–60°): breathing, eating, aspiration reduction
-
High Fowler’s (60–90°): NG insertion, maximal lung expansion
-
Supine: flat; protect pressure points
-
Prone: ARDS oxygenation; monitor closely
-
Sims’: rectal procedures; comfort/rest
Sleep hygiene
-
Quiet, dim lights, cluster care, cool room, limit evening caffeine, comfortable bedding
Pain management
-
Non-pharm: repositioning, heat/cold, massage, relaxation, music
-
Pharm: acetaminophen, NSAIDs, opioids (as prescribed); match to pain type; monitor effects
Vital Signs & Monitoring
Normal adult ranges
-
Temp: 97.8–99.1°F (36.5–37.3°C)
-
Pulse: 60–100 bpm
-
Respirations: 12–20/min
-
BP: <120/80 mmHg
-
SpO₂: 95–100%
-
Pain: 0–10 scale (patient-reported)
Pro tips
-
Compare to baseline; note meds/activity/pain
-
Report clinically significant changes promptly
-
Document time and relevant context
Documentation (the 5 C’s)
Clear • Concise • Complete • Correct • Current
-
Use approved abbreviations only
-
Chart subjective (“patient states…”) and objective (measurable data)
-
Be specific and timely; never chart for others
-
Correct errors per policy (no white-out)
-
Remember: “If it wasn’t documented, it wasn’t done.”
Patient Education (teach-back = gold standard)
-
Ask patients to repeat instructions in their own words
-
Avoid jargon; match literacy level; provide written reinforcement
-
Consider culture/language; use interpreters (not family)
-
Cover meds (name, purpose, dose, timing, side effects), treatments, warning signs, follow-up, and lifestyle changes
Delegation (safe, scope-aligned)
RN: initial assessments, teaching, evaluation, care plans, IV pushes (per policy), supervision
LPN/LVN: stable patients, routine meds (no IV push where restricted), wound care, data collection
UAP/CNA: ADLs, hygiene, stable vitals, ambulation, positioning, feeding
Five Rights of Delegation: Right Task, Circumstances, Person, Direction/Communication, Supervision/Evaluation
Do NOT delegate: unstable patients, nursing judgment, first-time assessments, teaching, sterile procedures (to UAP), meds (to UAP)
Priority setting & clinical reasoning
-
ABCs first; safety always
-
Acute > chronic, unstable > stable, new onset > expected
-
Ask: What’s the primary concern? What’s the worst likely complication? Which action has the greatest immediate impact on safety?
High-yield internal reads
Quick practice prompts (NCLEX Fundamentals)
-
New confused patient trying to get up unassisted. First action?
-
TB rule-out arrives on the unit. Room & PPE?
-
Post-op day 1, BP 88/54, HR 124, cool/clammy. Priority?
-
Family asks to translate complex discharge teaching. Best response?
-
UAP asks to record vitals on a fresh post-op with epidural. Delegate? Why/why not?
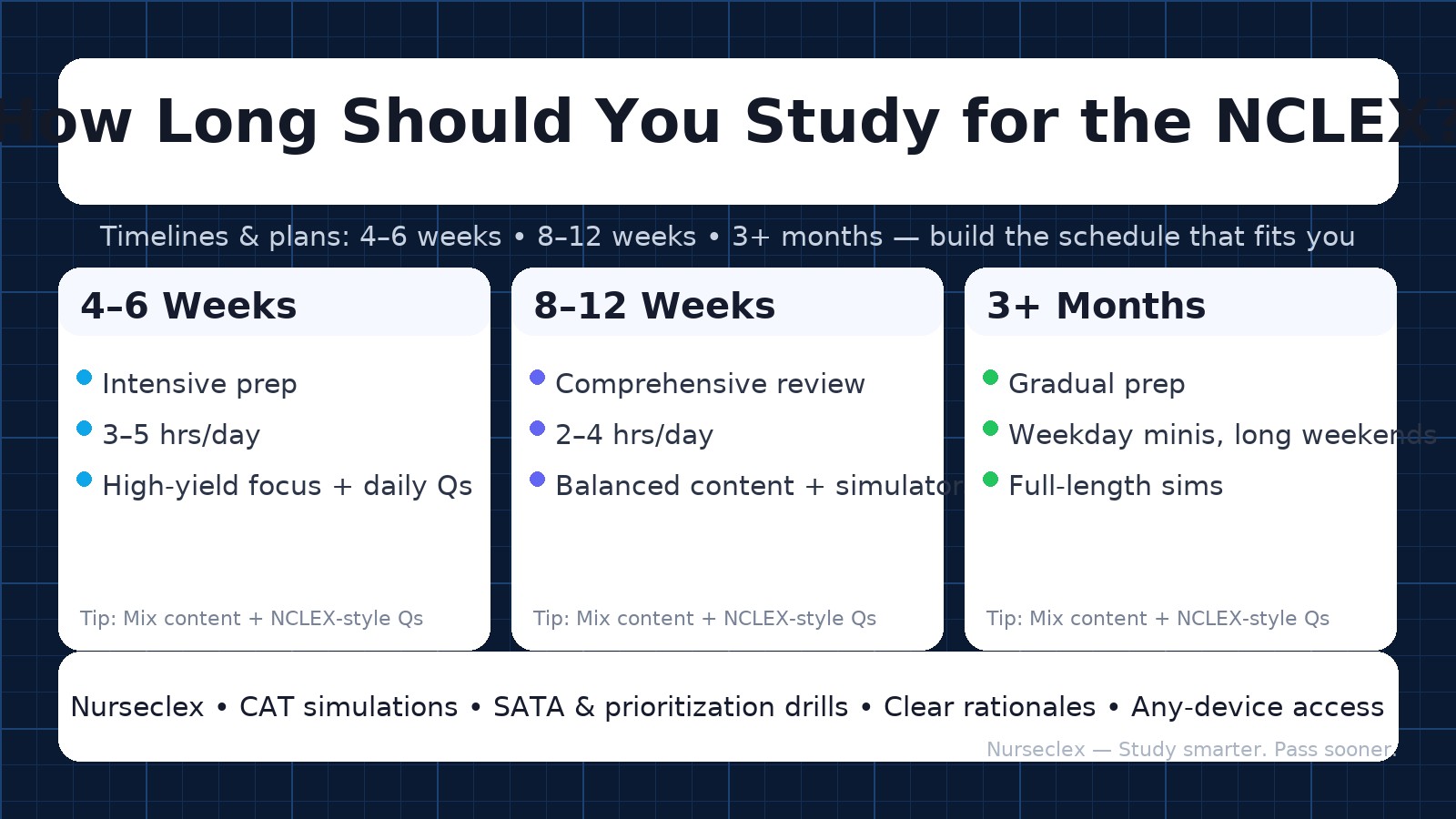
How to use this guide
-
Skim each checklist, then practice 50–75 NCLEX-style questions daily.
-
Revisit weak areas with teach-back and quick drills.
-
Finish with a timed fundamentals block to build stamina and pacing.
Nurseclex — study smarter, practice confidently, and pass the NCLEX on your first attempt