Quick definition (read this first)
Critical thinking is how you analyze information and make sense of it.
Clinical judgment is how you use that thinking to make safe, prioritized patient-care decisions.
On the NGN/NCLEX, clinical judgment is what gets scored—often step by step.
New to NGN? See the NCSBN overviews for the Clinical Judgment Model and the Next Generation NCLEX.
Clinical judgment vs critical thinking — side by side
| Dimension | Critical Thinking (CT) | Clinical Judgment (CJ) |
|---|---|---|
| Scope | Broad reasoning skills | Patient-specific decisions |
| On exam | Supports your thinking | The part that’s scored |
| Method | Tools: analysis, inference, compare/contrast | CJM steps: recognize → analyze → prioritize → solutions → action → evaluate |
| Output | Better ideas | Safer first actions and follow-ups |
The phrase clinical judgment vs critical thinking shows up on many study guides. Use this table to separate the two fast.
The Clinical Judgment Model (CJM) in 90 seconds
-
Recognize cues — Pull relevant data (vitals, labs, symptoms, trends).
-
Analyze cues — Cluster findings. Decide what they mean.
-
Prioritize hypotheses — Rank by danger and likelihood (ABCs, safety, stability, time).
-
Generate solutions — List safe, effective interventions.
-
Take action — Do the best first step.
-
Evaluate outcomes — Reassess. Did it work? What’s next?
Exam tip: Some items target one step. Answer for that step. Do not treat during “recognize cues.”
How critical thinking powers each step
-
Analysis & inference → Analyze cues. You separate noise from signal.
-
ABCs / safety / stability → Prioritize hypotheses. You choose what matters now.
-
Knowledge + dosage math → Generate solutions. You pick safe meds and actions.
-
Metacognition → Evaluate outcomes. You check bias and confirm trends.
Bottom line: Critical thinking is the engine; clinical judgment is the track the exam scores.
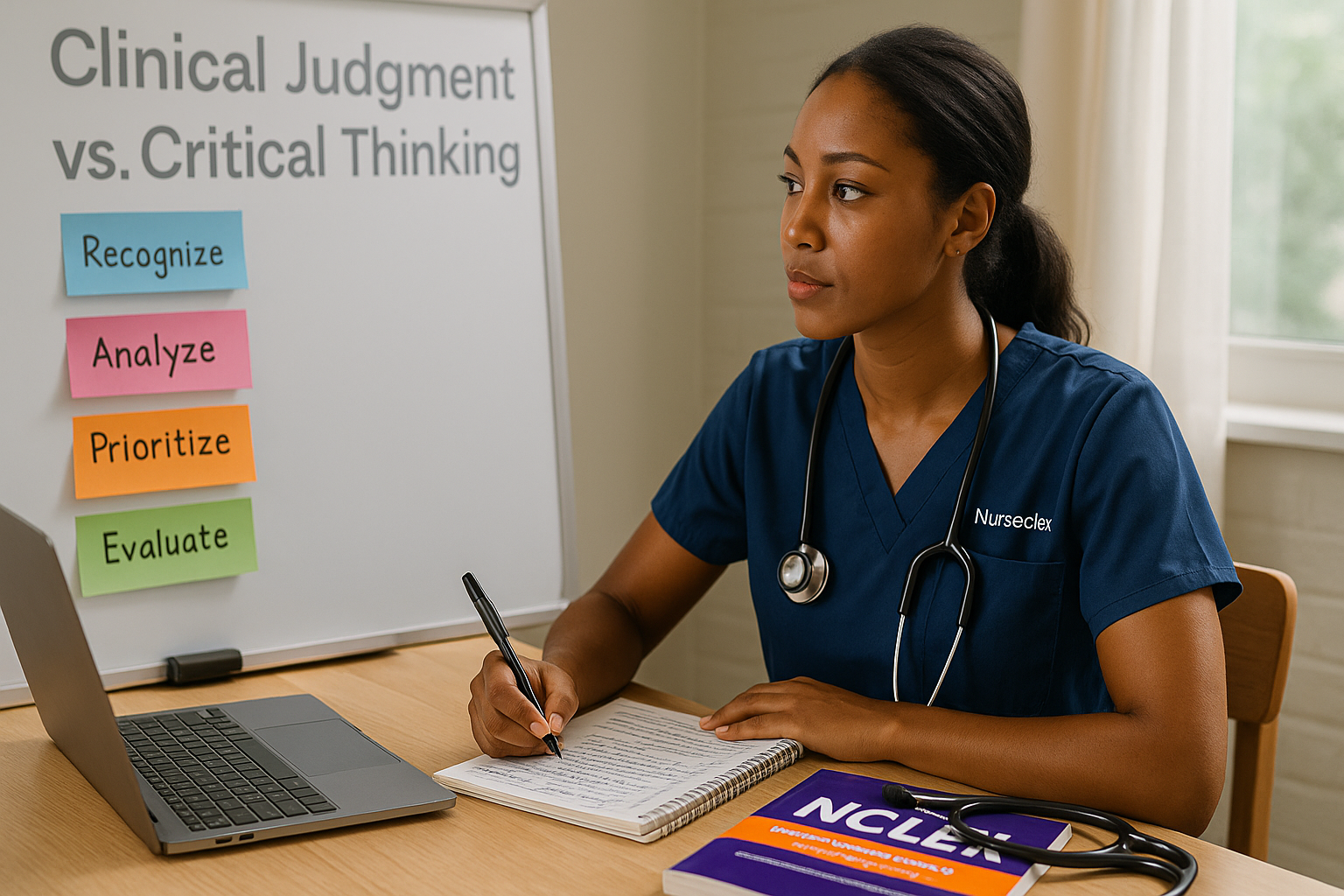
Image: Where the score comes from
Alt: “Clinical judgment vs critical thinking diagram with CJM steps and scoring focus”
Exam-day moves that win points
-
Think in steps. If the task is cues, don’t jump to treatment.
-
Use ABCs + Safety + Stability + Time-sensitive to rank choices.
-
Bank partial credit. Remove unsafe options first; choose all safe components you’re sure about.
-
Scan for trends before you “evaluate outcomes.”
Practice next:
Mini-case 1 (Cardio): DVT risk after surgery
Stem: POD1 abdominal surgery. HR 118, BP 100/64, RR 24, SpO₂ 92% RA, temp 38.5 °C, pain 7/10, calf tenderness RLE.
Apply CJM:
-
Recognize cues: tachycardia, low-normal BP, low SpO₂, fever, unilateral calf tenderness.
-
Analyze: cluster → VTE/DVT; risk of PE.
-
Prioritize hypotheses: VTE risk outranks atelectasis or routine pain.
-
Generate solutions: bed rest, notify provider, confirm anticoagulation orders, prep imaging; do not massage limb.
-
Take action: implement safety-first steps before ambulation.
-
Evaluate: monitor SpO₂, chest pain, dyspnea; reassess vitals.
Common traps: “Ambulate hourly” (unsafe with suspected DVT). “IS first” (not the priority).
Mini-case 2 (Resp): COPD exacerbation
Stem: RR 30, accessory muscles, SpO₂ 88% on 2 L NC, wheezes, anxious, 3–4-word sentences.
-
If the item asks “Which findings need immediate follow-up?” → pick work of breathing and hypoxemia.
-
If the next item asks “Which action first?” → escalate oxygen per protocol (↑ flow or device), high-Fowler’s, prep bronchodilator.
-
Trap: Teaching now. Stabilize first; teach later.
10 quick checks (fast self-audit)
-
Is this about cues or actions?
-
Anyone hypoxic, bleeding, or neurologically worsening?
-
Any unsafe or out-of-scope option (e.g., UAP gives meds)?
-
Unstable or time-sensitive signs present?
-
Is there partial credit? Lock safe components.
-
Do you see a trend (SpO₂ down, UO down)?
-
Orders say titrate to effect—do you know start ranges and monitoring?
-
After action, what will you reassess?
-
Can you delegate safely? Only stable, predictable tasks to UAP; LPN scope varies.
-
Does the option treat the cause and protect the patient now?
Practice: Name the CJM step
-
“Select all relevant findings for suspected GI bleed.” → Recognize cues
-
“Which problem is the priority?” → Prioritize hypotheses
-
“Which nursing action is best to do first?” → Take action
Image: Clinical judgment vs critical thinking (quick card)
Alt: “Side-by-side card labeling critical thinking tools vs clinical judgment steps”
FAQs
Is clinical judgment the same as critical thinking?
No. Critical thinking is broad. Clinical judgment is its bedside use—and it’s what NGN measures.
How is CJM tested on NGN?
Through case sets. Some items focus on relevant cues. Others test prioritization or actions. Many award partial credit.
What frameworks help with prioritization?
ABCs, safety first, stable vs unstable, and time-sensitive problems (oxygenation, perfusion, neuro).
How often should I use the exact phrase “clinical judgment vs critical thinking”?
Use it naturally: in the title, meta, one H2, the body, and one image alt or internal-link anchor.
What to read next
Authoritative resources: