You’ve collected the signals—now make them work. Analysis and prioritization is where cue clusters become one clear problem and a safe, first action. Use the simple rules below to sort what matters now from what can wait.
Need a refresher on finding the right signals? Start with: Cue Recognition Patterns. For the big-picture thinking flow, see Clinical Judgment vs Critical Thinking.
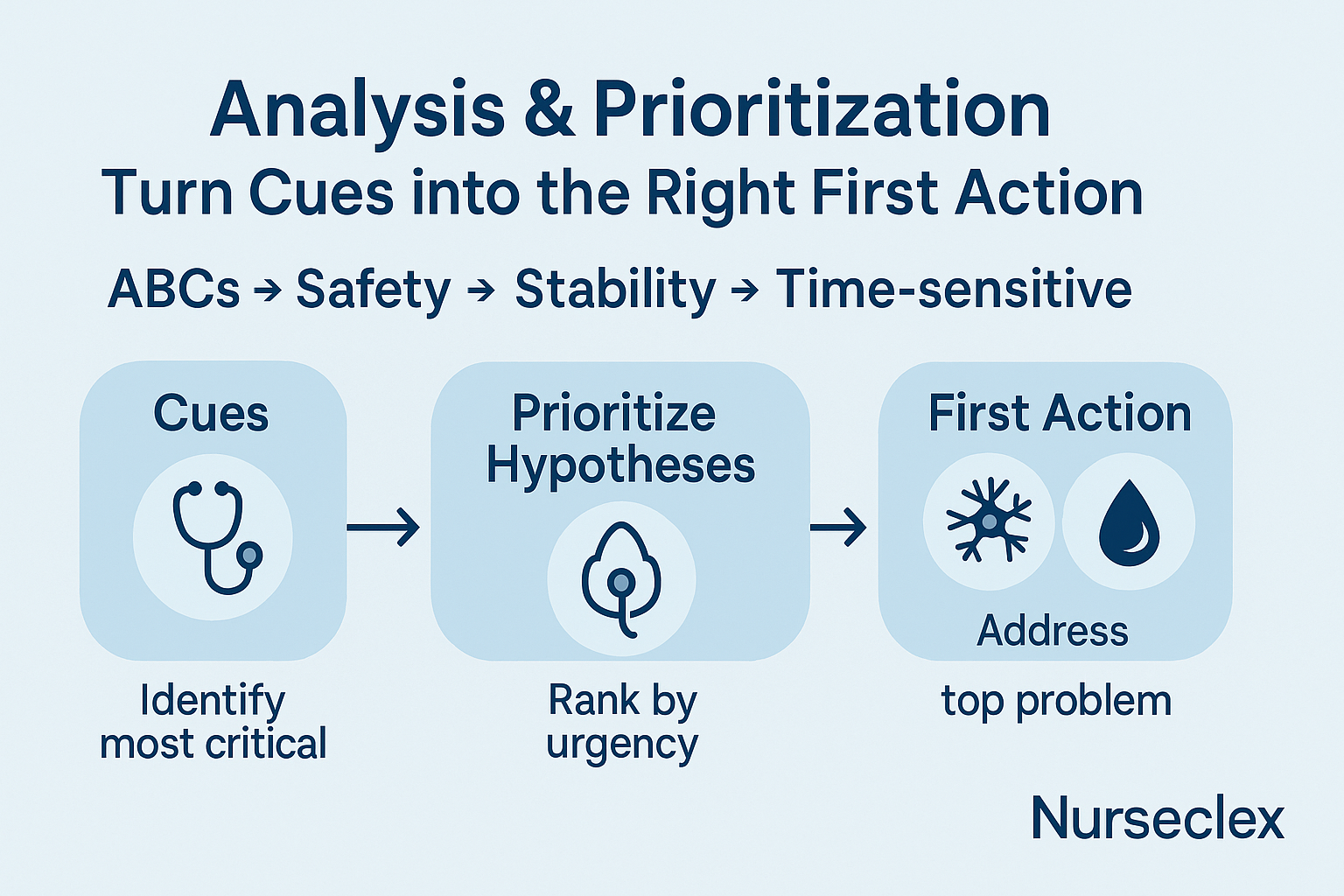
Image: The thinking path at a glance
Alt: “Analysis and prioritization flow: summarize cues → system → ABCs → safety/stability → time-sensitive → priority problem”
A 6-step mini-flow you can memorize
-
Summarize the cue cluster in one sentence.
-
Name the body system(s) most involved.
-
Apply ABCs (airway/oxygenation first).
-
Screen safety & stability (unstable > stable).
-
Check time-sensitive issues (hypoglycemia, stroke, sepsis, hemorrhage).
-
State one priority problem—the thing your next action must address.
Keep it short. Analysis and prioritization is a decision, not a paragraph.
The rule stack (use in order)
-
ABCs: oxygenation/airway beats everything.
-
Safety: stop bleeding, stop seizures, protect airway, prevent falls.
-
Stability: unstable (rapid changes, new neuro deficits, shock signs) outranks stable.
-
Time-sensitive: treat what is reversible now (e.g., low glucose) before longer workups.
-
Least invasive first: when safe options tie, start with the least invasive effective step.
Worked comparisons you’ll actually see
Chest pain vs postoperative pain
-
Cues: Diaphoresis, pressure-like chest pain vs incisional pain 8/10 with stable vitals.
-
Priority: Perfusion risk (possible ACS) outranks routine pain control.
New confusion vs chronic back pain
-
Cues: New confusion + fever 38.8 °C vs chronic back pain 6/10.
-
Priority: Acute neuro change with infection signs wins.
Falling SpO₂ vs elevated but stable BP
-
Cues: SpO₂ 93 → 90 → 88 on same device vs BP 160/92 unchanged for 24h.
-
Priority: Oxygenation trend wins.
Mini-case 1: Stroke or sugar?
Stem (short): Sudden slurred speech, right-arm weakness, BG 48 mg/dL, last known well 20 min ago.
-
Summarize cues: Focal neuro deficits + severe hypoglycemia.
-
Rule stack: ABCs ok? → Time-sensitive hypoglycemia is rapidly reversible and life-threatening.
-
Priority problem: Hypoglycemia (treat now), then stroke workup.
Learn the scoring strategy you’ll use on multi-part items: NGN Partial-Credit Scoring.
Mini-case 2: COPD flare—what’s first?
Stem (short): RR 30, 3–4 word sentences, SpO₂ 88% on 2 L, wheezes, anxious.
-
Summarize cues: Worsening oxygenation and work of breathing.
-
Priority problem: Impaired oxygenation.
-
Safest first step (next item): Escalate O₂ per protocol and position high-Fowler’s before education or long teaching moments.
When the stem shows a downtrend, treat it like this: Trend Items: Safe vs Improving vs Deteriorating.
Image: Priority ties—how to break them
Alt: “Analysis and prioritization tiebreakers: ABCs → safety → stability → time-sensitive → least invasive”
Common mistakes (and the fix)
-
Treating comfort before safety.
Fix: Ask “Does this affect airway, perfusion, or neuro right now?” -
Choosing the most detailed option.
Fix: Detail isn’t safety. Pick the safest effective first action. -
Forgetting trends.
Fix: Re-scan for direction (SpO₂, neuro checks, urine output) before deciding. -
Confusing “common” with “priority.”
Fix: A common problem can wait if a life threat is present.
Quick drills (10 seconds each)
-
Pick the priority problem:
Cues: fever 39 °C, rigid neck, photophobia.
→ Suspected meningitis (neuro infection risk). -
Break the tie:
Cues: BG 58 mg/dL and new unilateral weakness.
→ Treat hypoglycemia first (time-sensitive), then evaluate neuro deficit. -
Choose what matters now:
Cues: post-op 8 hours, BP 96/60 (baseline 130/80), HR 118, cool clammy skin.
→ Shock/perfusion concern > routine pain control.
One-page checklist (print this)
-
I summarized cues into one sentence
-
I applied ABCs first
-
I screened safety and stability
-
I checked time-sensitive conditions
-
I named one priority problem that drives the next action
FAQs
Do I ever pick pain first?
Yes—when unmanaged pain creates a safety risk (e.g., chest pain with perfusion red flags, or severe post-op pain causing hypoventilation). Otherwise, oxygenation/perfusion wins.
What if two answers are safe?
Choose the option that is most immediate and least invasive while addressing the priority problem.
How do I get faster at analysis and prioritization?
Practice short cases with a timer, then review why your priority won under ABCs, safety, stability, time.
Keep going
Authoritative resource:
NCSBN explanations of clinical judgment and NGN item formats provide deeper context for how these decisions are tested.