One-sentence definition (featured snippet)
Trend items NGN test whether you act on the direction of change—on the same device and settings—instead of reacting to a single number.
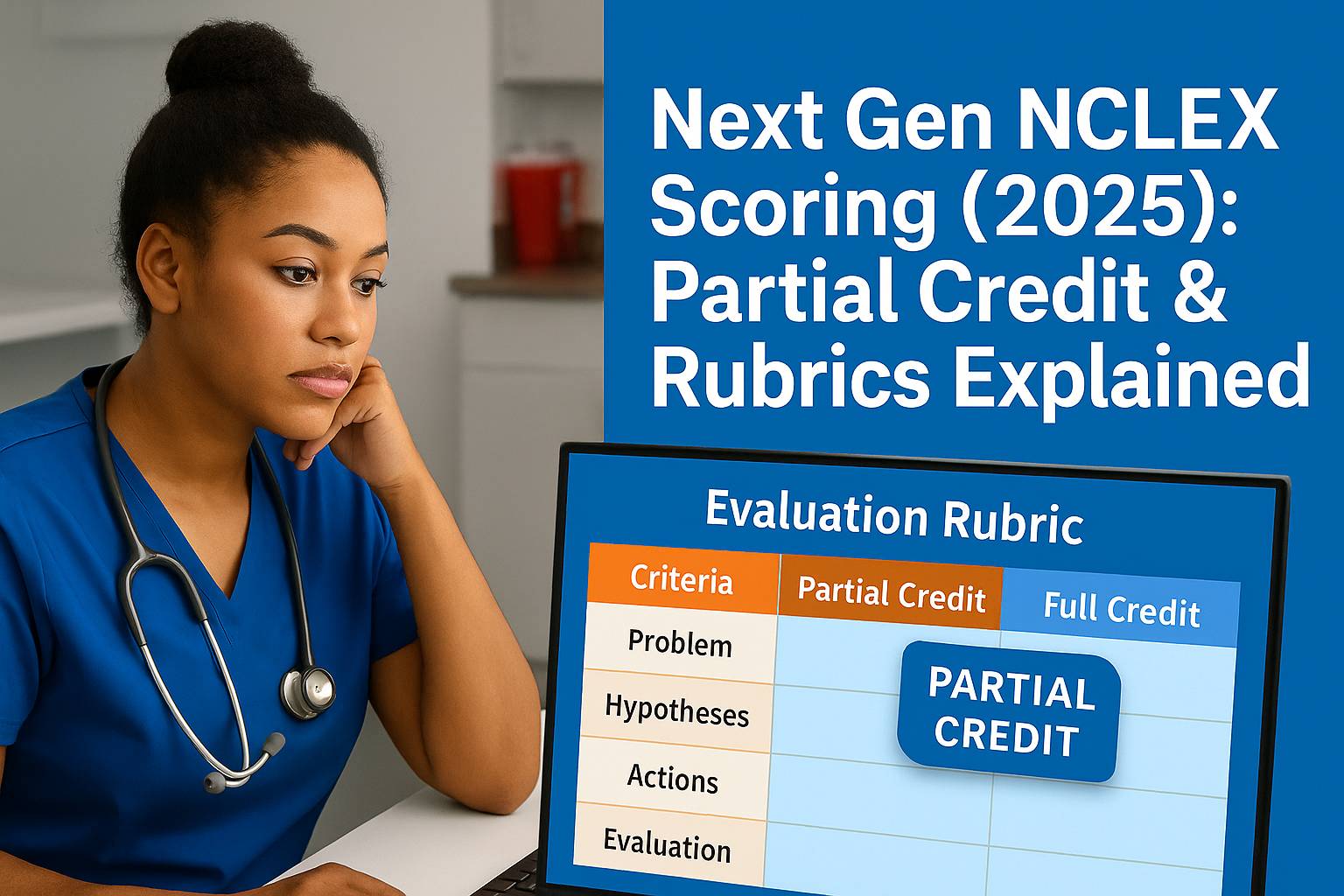
New to the NGN flow? Brush up on Cue Recognition and Analysis & Prioritization. Also see NGN Partial Credit.
The “same device” rule (non-negotiable)
Only call it a trend if values come from the same device, same settings, and same context.
Changed from room air to 2 L NC? That’s a context change, not a clean trend. Re-establish baseline or compare like with like.
Why it matters: Trend items NGN reward clean comparisons. Mixed sources can mislead and push you toward unsafe picks.
Three rapid trend sets you’ll see
1) Oxygenation trend
-
SpO₂: 93 → 90 → 88 on 2 L nasal cannula
-
Other cues: RR rising; accessory muscles
-
Safest first action: Escalate oxygen per protocol (↑ flow or switch device) and position high-Fowler’s.
-
Avoid: Teaching first. Stabilize before education.
2) Neuro trend
-
Neuro checks: new unequal pupils after head injury
-
Safest first action: Notify provider STAT; protect airway; keep head midline; prepare for imaging.
-
Avoid: Non-urgent tasks. This is time-sensitive.
3) Renal/perfusion trend
-
Urine output: 50 → 30 → 20 mL/hr on vasoactive drip
-
Other cues: cool, clammy skin
-
Safest first action: Suspect perfusion problem; notify provider; assess hemodynamics; follow protocol.
-
Avoid: Comfort-only actions that do not treat cause.
Device escalation (quick table)
| Situation | Current | When to escalate | Safer next step |
|---|---|---|---|
| SpO₂ 93→90→88 with ↑ WOB | 2 L NC | Downtrend on same device | Increase flow or switch to Venturi/non-rebreather per protocol; high-Fowler’s |
| Rising CO₂ with fatigue | Simple mask | Hypercapnia worsening | Evaluate Venturi/BiPAP per orders; monitor ABGs |
| Neuro decline | Neuro checks | New unequal pupils | Notify provider STAT; protect airway; prepare for imaging |
Use this table on trend items NGN when deciding device changes or escalation.
Numbers that move the needle
-
SpO₂ ≤ 90% on the same device/settings → escalate oxygen now.
-
MAP < 65 mmHg despite fluids → escalate per protocol.
-
Urine output < 30 mL/hr with cool, clammy skin → treat perfusion risk first.
Pro tip: On trend items NGN, direction + danger beats a single “interesting” value.
Reassess like a pro (after your action)
After you intervene, recheck four things:
-
Device/flow (what is the patient on now?)
-
Vitals trend (did direction change?)
-
Symptoms (work of breathing, neuro status, perfusion signs)
-
One target metric (e.g., SpO₂ ≥ 92%, MAP ≥ 65, UO ≥ 30 mL/hr)
If the trend does not improve, escalate again using policy and orders.
Quick checklist (print this)
-
Same device/settings confirmed
-
ABCs and neuro prioritized
-
Safest first action chosen (least invasive that works)
-
Reassessed direction and key metric
-
Documented effect and next steps
Common mistakes (and fixes)
-
Single-number trap: Treating one low value like a trend.
-
Fix: Look for 3 points in one direction under the same conditions.
-
-
Context blindness: Ignoring device type and flow.
-
Fix: Tie every saturation to device + settings.
-
-
Teaching too soon:
-
Fix: Stabilize first. Teach when safe.
-
Image (hero)
File: hero-trend-items.jpg
Alt: “Line chart card showing a declining oxygen trend with safety reminders for trend items NGN”
Internal links (keep readers moving)
FAQs (for on-page SEO)
Q: How many points make a trend?
A: Three values in one direction, under the same device and settings, is a safe rule for trend items NGN.
Q: Do I ever pick pain control first?
A: Only when oxygenation, perfusion, and neuro threats are absent. Safety first.
Q: What if device settings changed between readings?
A: That is not a clean trend. Compare like with like, or recheck.